Overview

?Life begins at 40,? goes an old quote, ?and so do fallen arches.? It?s time to toss that negative idea out the window and get the real facts on fallen arches and what you can do about them. We have all seen what our footprints look like as we walked across sand or left a water trail after getting out of the bathtub. The narrow part of the footprint is where your natural arch exists. What gives you that arch are tendons that pull together to create an upward curve. When your tendons are not properly pulling together, you start to lose that natural arch. This condition is known as flat foot or fallen arch.
Causes
Having low or no arches is normal for some people. In these cases, flat feet are usually inherited and the feet are fairly flexible. Occasionally, flat feet can be caused by an abnormality that develops in the womb, such as a problem with a joint or where two or more bones are fused together. This is known as tarsal coalition and results in the feet being flat and stiff. Flat feet that develop in later life can be caused by a condition that affects the joints, such as arthritis, or an injury to a muscle, tendon or joint in the foot. Conditions that affect the nervous system (brain and spinal cord) can also cause the arches to fall. Over time, the muscles gradually become stiffer and weaker and lose their flexibility. Conditions where this can occur include cerebral palsy, spina bifida and muscular dystrophy. Adult-acquired flat feet often affect women over 40 years of age. It often goes undiagnosed and develops when the tendon that supports the foot arch gradually stretches over time. It's not fully understood what causes the tendon to become stretched, but some experts believe that wearing high heels and standing or walking for long periods may play a part. Obesity, high blood pressure (hypertension) and diabetes are all risk factors. Recent research has found a link with changes to the tendon in the foot and an increase in a type of protein called proteolytic enzyme. These enzymes can break down some areas of the tendon, weakening it and causing the foot arch to fall. Similar changes are also seen in other conditions, such as Achilles tendonitis. This could have important implications for treating flat feet because medication that specifically targets these enzymes could provide an alternative to surgery. However, further research is needed and this type of treatment is thought to be about 10 to 15 years away.
Symptoms
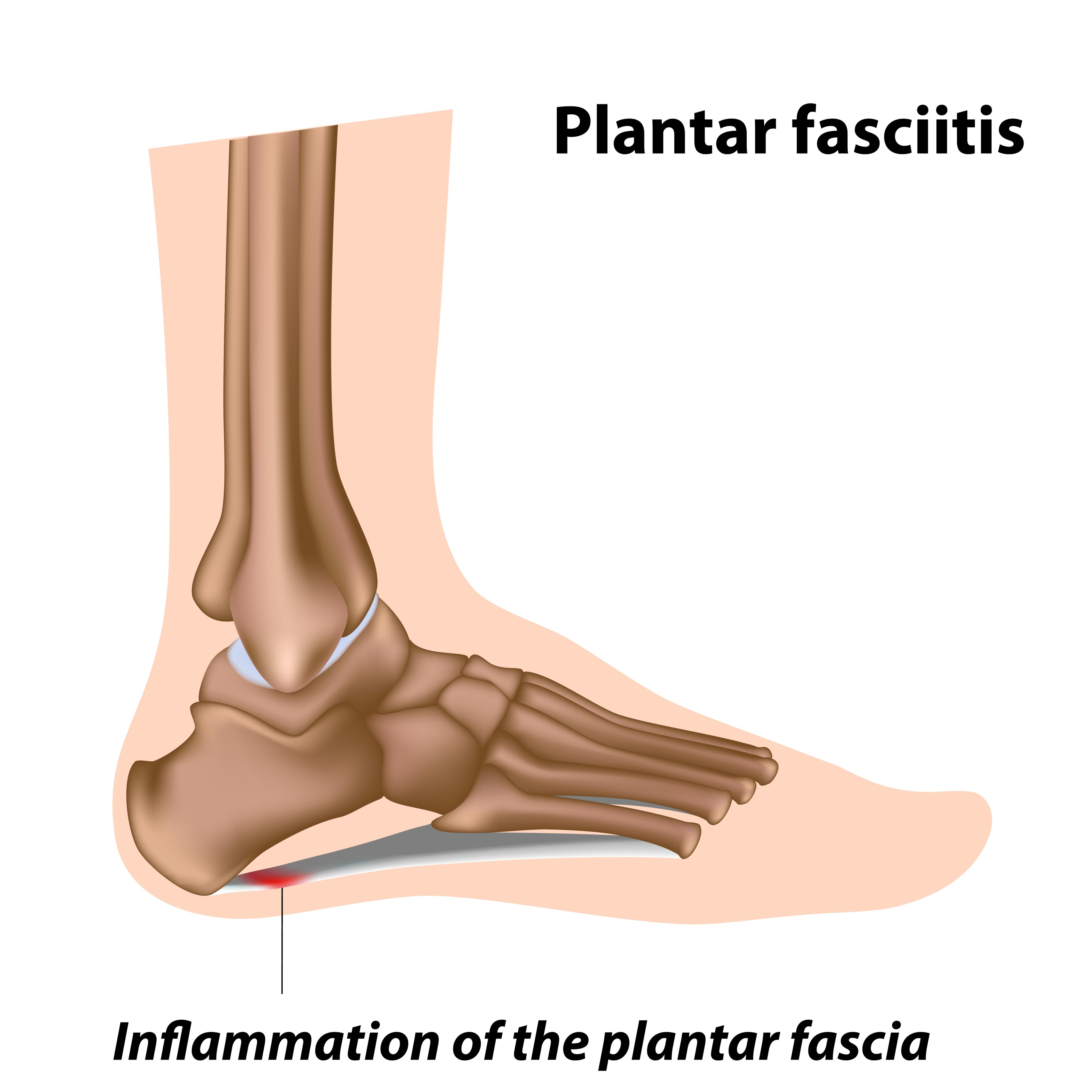
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in the adult with a rigid flat foot. An easy and traditional home diagnosis is the "wet footprint" test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
How do you get an arch in your foot?
Non Surgical Treatment
Switch activities for a little while. If you?re a super athlete, you don?t want to hear that you need to take a break, but there?s no way around it. You need to lay off the high impact sports like basketball, tennis and running. Don?t panic-there?s no shortage of alternatives. Find a high school track that?s open to the public and try going for a run. Many athletic programs use spongy synthetic materials to pave tracks instead of concrete. This is much easier on all the joints and tendons, not only in your feet but your legs and ankles. You can also try running on dirt trails or stable grassy areas. Take up swimming for a little while. This is actually an ideal activity for your arches. The buoyancy of water takes weight off our feet, but still allows for aerobic activity. Many gyms and activity centers also offer various water sport classes. In no time flat, you?ll be on your way to healthier feet.
Surgical Treatment
.JPG)
Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

?Life begins at 40,? goes an old quote, ?and so do fallen arches.? It?s time to toss that negative idea out the window and get the real facts on fallen arches and what you can do about them. We have all seen what our footprints look like as we walked across sand or left a water trail after getting out of the bathtub. The narrow part of the footprint is where your natural arch exists. What gives you that arch are tendons that pull together to create an upward curve. When your tendons are not properly pulling together, you start to lose that natural arch. This condition is known as flat foot or fallen arch.
Causes
Having low or no arches is normal for some people. In these cases, flat feet are usually inherited and the feet are fairly flexible. Occasionally, flat feet can be caused by an abnormality that develops in the womb, such as a problem with a joint or where two or more bones are fused together. This is known as tarsal coalition and results in the feet being flat and stiff. Flat feet that develop in later life can be caused by a condition that affects the joints, such as arthritis, or an injury to a muscle, tendon or joint in the foot. Conditions that affect the nervous system (brain and spinal cord) can also cause the arches to fall. Over time, the muscles gradually become stiffer and weaker and lose their flexibility. Conditions where this can occur include cerebral palsy, spina bifida and muscular dystrophy. Adult-acquired flat feet often affect women over 40 years of age. It often goes undiagnosed and develops when the tendon that supports the foot arch gradually stretches over time. It's not fully understood what causes the tendon to become stretched, but some experts believe that wearing high heels and standing or walking for long periods may play a part. Obesity, high blood pressure (hypertension) and diabetes are all risk factors. Recent research has found a link with changes to the tendon in the foot and an increase in a type of protein called proteolytic enzyme. These enzymes can break down some areas of the tendon, weakening it and causing the foot arch to fall. Similar changes are also seen in other conditions, such as Achilles tendonitis. This could have important implications for treating flat feet because medication that specifically targets these enzymes could provide an alternative to surgery. However, further research is needed and this type of treatment is thought to be about 10 to 15 years away.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in the adult with a rigid flat foot. An easy and traditional home diagnosis is the "wet footprint" test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
How do you get an arch in your foot?
Non Surgical Treatment
Switch activities for a little while. If you?re a super athlete, you don?t want to hear that you need to take a break, but there?s no way around it. You need to lay off the high impact sports like basketball, tennis and running. Don?t panic-there?s no shortage of alternatives. Find a high school track that?s open to the public and try going for a run. Many athletic programs use spongy synthetic materials to pave tracks instead of concrete. This is much easier on all the joints and tendons, not only in your feet but your legs and ankles. You can also try running on dirt trails or stable grassy areas. Take up swimming for a little while. This is actually an ideal activity for your arches. The buoyancy of water takes weight off our feet, but still allows for aerobic activity. Many gyms and activity centers also offer various water sport classes. In no time flat, you?ll be on your way to healthier feet.
Surgical Treatment
.JPG)
Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.


 Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.
Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.






 Symptoms
Symptoms Prevention
Prevention The Achilles tendon is found in the back of the leg above the heel, and is the largest tendon in the body. It connects the calf muscles to the heel bone and is used when walking, running and jumping. A rupture of the tendon is a tearing and separation of the tendon fibers. When a rupture of the tendon occurs, the tendon can no longer perform its normal function. A common issue related to a tear is the inability to point your toe. Causes The most common cause of a ruptured Achilles' tendon is when too much stress is placed through the tendon, particularly when pushing off with the foot. This may happen when playing sports such as football, basketball or tennis where the foot is dorsiflexed or pushed into an upward position during a fall. If the Achilles' tendon is weak, it is prone to rupture. Various factors can cause weakness, including corticosteroid medication and injections, certain diseases caused by hormone imbalance and tendonitis. Old age can also increase the risk of Achilles' tendon rupture. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis The diagnosis is usually made on the basis of symptoms, the history of the injury and a doctor's examination. The doctor may look at your walking and observe whether you can stand on tiptoe. She/he may test the tendon using a method called Thompson's test (also known as the calf squeeze test). In this test, you will be asked to lie face down on the examination bench and to bend your knee. The doctor will gently squeeze the calf muscles at the back of your leg, and observe how the ankle moves. If the Achilles tendon is OK, the calf squeeze will make the foot point briefly away from the leg (a movement called plantar flexion). This is quite an accurate test for Achilles tendon rupture. If the diagnosis is uncertain, an ultrasound or MRI scan may help. An Achilles tendon rupture is sometimes difficult to diagnose and can be missed on first assessment. It is important for both doctors and patients to be aware of this and to look carefully for an Achilles tendon rupture if it is suspected. Non Surgical Treatment The most widely used method of non-surgical treatment involves the use of serial casting with gradual progression from plantar flexion to neutral or using a solid removable boot with heel inserts to bring the ends of the tendon closer together. The advantage of a solid removable boot is that it allows the patient to begin early motion and is removable. Wide variability exists among surgeons in regards to the period of absolute immobilization, initiating range of motion exercises, and progression of weight bearing status.
The Achilles tendon is found in the back of the leg above the heel, and is the largest tendon in the body. It connects the calf muscles to the heel bone and is used when walking, running and jumping. A rupture of the tendon is a tearing and separation of the tendon fibers. When a rupture of the tendon occurs, the tendon can no longer perform its normal function. A common issue related to a tear is the inability to point your toe. Causes The most common cause of a ruptured Achilles' tendon is when too much stress is placed through the tendon, particularly when pushing off with the foot. This may happen when playing sports such as football, basketball or tennis where the foot is dorsiflexed or pushed into an upward position during a fall. If the Achilles' tendon is weak, it is prone to rupture. Various factors can cause weakness, including corticosteroid medication and injections, certain diseases caused by hormone imbalance and tendonitis. Old age can also increase the risk of Achilles' tendon rupture. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis The diagnosis is usually made on the basis of symptoms, the history of the injury and a doctor's examination. The doctor may look at your walking and observe whether you can stand on tiptoe. She/he may test the tendon using a method called Thompson's test (also known as the calf squeeze test). In this test, you will be asked to lie face down on the examination bench and to bend your knee. The doctor will gently squeeze the calf muscles at the back of your leg, and observe how the ankle moves. If the Achilles tendon is OK, the calf squeeze will make the foot point briefly away from the leg (a movement called plantar flexion). This is quite an accurate test for Achilles tendon rupture. If the diagnosis is uncertain, an ultrasound or MRI scan may help. An Achilles tendon rupture is sometimes difficult to diagnose and can be missed on first assessment. It is important for both doctors and patients to be aware of this and to look carefully for an Achilles tendon rupture if it is suspected. Non Surgical Treatment The most widely used method of non-surgical treatment involves the use of serial casting with gradual progression from plantar flexion to neutral or using a solid removable boot with heel inserts to bring the ends of the tendon closer together. The advantage of a solid removable boot is that it allows the patient to begin early motion and is removable. Wide variability exists among surgeons in regards to the period of absolute immobilization, initiating range of motion exercises, and progression of weight bearing status.  Surgical Treatment This condition should be diagnosed and treated as soon as possible, because prompt treatment probably improves recovery. You may need to be referred urgently to see a doctor in an orthopaedic department or accident and emergency department. Meanwhile, if a ruptured Achilles tendon is suspected, you should not put any weight on that foot, so do not walk on it at all. A new piece of research found that surgery and conservative treatment actually gave equally good results, when patients were also given early mobilisation treatment using a brace. If an operation is needed, there is a type of surgery called percutaneous, which uses smaller cuts than the traditional operation. This seems to reduce the risk of getting a wound infection. After surgery, a brace seems to be better than a plaster cast in terms of faster recovery and return to normal activities, a lower complication rate and patient preferences. Prevention Here are some suggestions to help to prevent this injury. Corticosteroid medication such as prednisolone, should be used carefully and the dose should be reduced if possible. But note that there are many conditions where corticosteroid medication is important or lifesaving. Quinolone antibiotics should be used carefully in people aged over 60 or who are taking steroids.
Surgical Treatment This condition should be diagnosed and treated as soon as possible, because prompt treatment probably improves recovery. You may need to be referred urgently to see a doctor in an orthopaedic department or accident and emergency department. Meanwhile, if a ruptured Achilles tendon is suspected, you should not put any weight on that foot, so do not walk on it at all. A new piece of research found that surgery and conservative treatment actually gave equally good results, when patients were also given early mobilisation treatment using a brace. If an operation is needed, there is a type of surgery called percutaneous, which uses smaller cuts than the traditional operation. This seems to reduce the risk of getting a wound infection. After surgery, a brace seems to be better than a plaster cast in terms of faster recovery and return to normal activities, a lower complication rate and patient preferences. Prevention Here are some suggestions to help to prevent this injury. Corticosteroid medication such as prednisolone, should be used carefully and the dose should be reduced if possible. But note that there are many conditions where corticosteroid medication is important or lifesaving. Quinolone antibiotics should be used carefully in people aged over 60 or who are taking steroids.
